 A new study entitled “Riluzole is a radio-sensitizing agent in an in vivo model of brain metastasis derived from GRM1 expressing human melanoma cells” shows that riluzole administration in animal models of melanoma brain metastasis can reduce tumor cell’s resistance to radiotherapy. The study was published in the journal Pigment Cell & Melanoma Research.
A new study entitled “Riluzole is a radio-sensitizing agent in an in vivo model of brain metastasis derived from GRM1 expressing human melanoma cells” shows that riluzole administration in animal models of melanoma brain metastasis can reduce tumor cell’s resistance to radiotherapy. The study was published in the journal Pigment Cell & Melanoma Research.
Melanoma is the deadliest form of skin cancer, with estimates of 76,100 new cases and 9,710 deaths during the year of 2014 in the United States alone, according to the National Cancer Institute, at the National Institutes of Health.
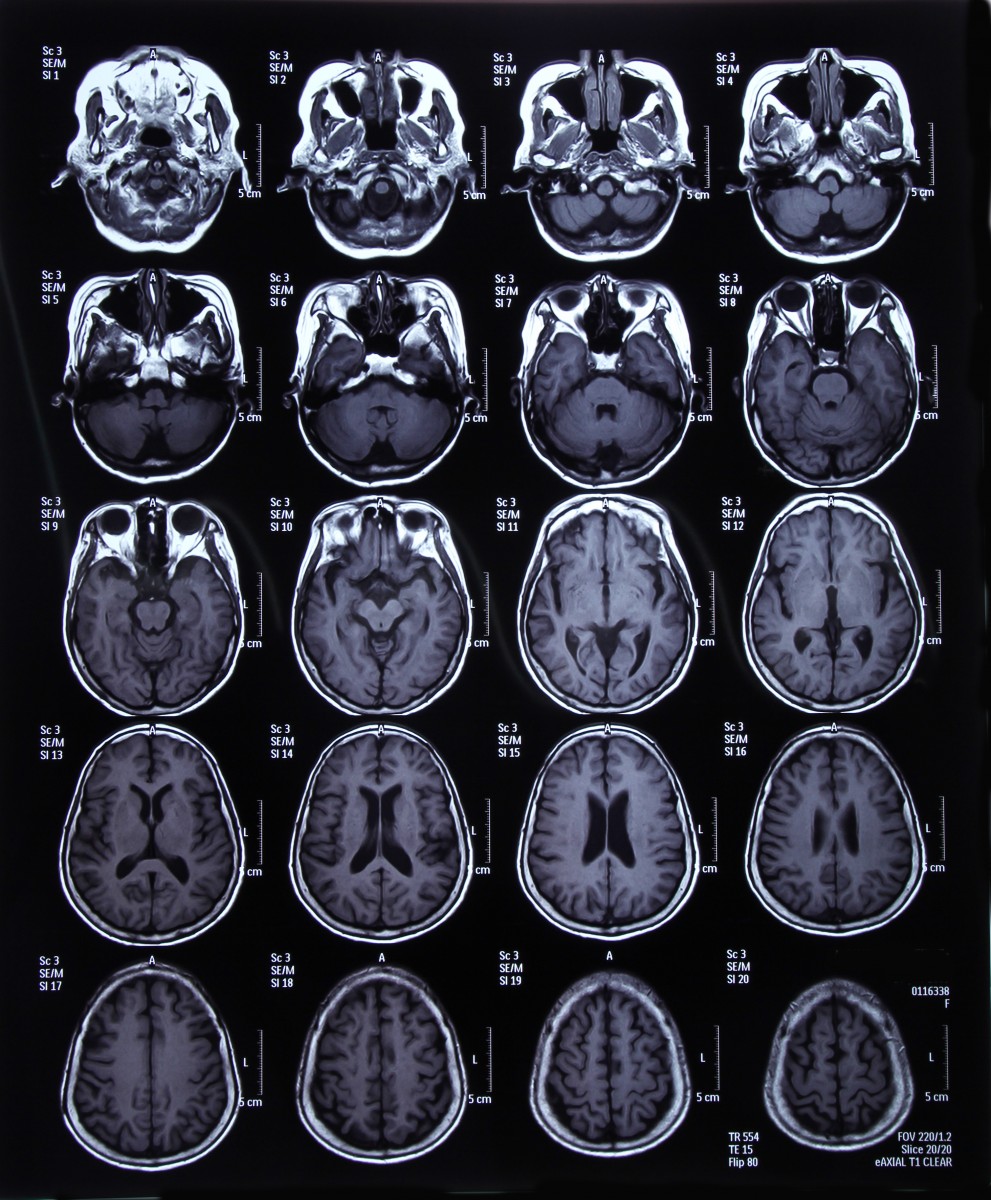
Patients with melanoma can not only exhibit resistance to current radiation therapy, but very often those with metastatic melanoma (approximately, 50% of patients) develop brain metastases. The underlying resistance is usually address by increasing radiation dosages, however, this approach is known to be highly toxic when delivered to the whole brain.
In this study, a team of researchers at the Rutgers Cancer Institute of New Jersey and Ernest Mario School of Pharmacy at Rutgers University studied human melanoma cells expressing a protein GRM1 (short for glutamate receptor metabotropic 1 and usually increased in melanoma) and its response to radiotherapy in combination with a GRM1-target drug, riluzole. This drug was approved by the United States Food and Drug Administration (FDA) as a therapy for Amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease. Its mode of action consists in blocking activation of the GRM1 protein.
The authors implanted GRM1-positive human melanoma cell xenografts (surgical graft of tissue) into mice and allowed brain metastasis to form. The mice were divided into four groups, each receiving a specific treatment – one group administered only the vehicle drug, dimethyl sulfoxide; a second group receiving both dimethyl sulfoxide and radiotherapy (weekly radiation dose of 4 Gy); a third group treated with daily doses of riluzole; and a fourth group treated with both riluzole (daily administration) and radiotherapy at 4 Gy.
[adrotate group=”1″]
The team observed a reduction in tumor growth in the brain of mice treated with both riluzole and radiation, when compared to all the other groups. Thus, the authors highlight riluzole administration renders melanoma cells more sensitive to radiation, and therefore may be a potential new drug to enhance radiotherapy for brain metastasis in melanoma patients.
Suzie Chen, PhD, Cancer Institute member and professor of chemical biology at the Ernest Mario School of Pharmacy and study leading author commented in a press release, “What this indicates is that riluzole sensitizes GRM1, helping these proteins act like a beacon for radiation so that only melanoma cells with the GRM1 protein will be targeted, sparing the rest of the brain and preserving the brain’s functionality.”
James S. Goydos, MD, director of the Melanoma and Soft Tissue Oncology Program at the Cancer Institute and professor of surgery at Rutgers Robert Wood Johnson Medical School, added “With approximately 50 percent of patients with melanoma developing brain metastasis and fewer than 13 percent of those patients surviving one year or more, identifying new therapies for this population is paramount. Because the GRM1 protein is also found in breast and prostate cancers, pre-treatment with riluzole before radiation for these particular cancers might also result in the same outcomes.”