 There is increasing evidence showing radiation therapy’s capacity to elicit strong anti-tumor responses through direct effects on tumor cells, such as immunogenic cell death and phenotypic change.
There is increasing evidence showing radiation therapy’s capacity to elicit strong anti-tumor responses through direct effects on tumor cells, such as immunogenic cell death and phenotypic change.
In a recent review article titled “Unlocking the Combination: Potentiation of Radiation-Induced Antitumor Responses with Immunotherapy”, published in the Radiation Research journal, Dr. Max M. Wattenberg, Laboratory of Tumor Immunology and Biology, Center for Cancer Research, National Cancer Institute, National Institutes of Health, Bethesda, Maryland, and colleagues, discussed the capacity of radiation therapy to induce antitumor immunity, along with the different effects of radiation on antigen-presenting cells (APCs) and cytotoxic T lymphocytes.
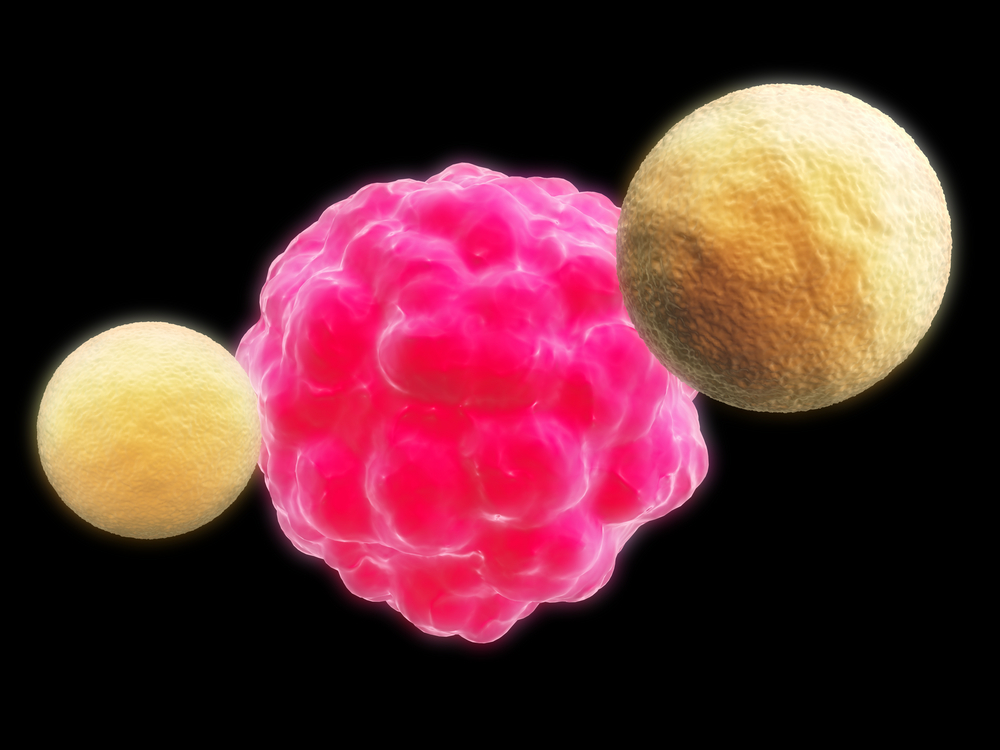
Radiation therapy can change the phenotype of cell surface receptors, including cell death receptors, tumor-associated antigens and adhesion molecules, allowing tumors cells to become more vulnerable to immune responses.
Usually, radiation therapy is used to destroy tumor cells or to modify the tumor/stroma with a curative of palliative purpose.
However, different cells within the same tumor commonly receive different amounts of radiation due to the limited dosage used to prevent healthy tissue damage. Nonetheless, even small doses of radiation can elicit strong immune responses by modifying tumor cells in a number of different ways.
The possibility of combining radiotherapy with immunotherapy allows physicians to use radiation-induced tumor cell death as a possible source of tumor antigens for immunotherapy and post-irradiation tumor cell modulation, allowing more effective immune cell access and improved sensitivity to T-cell killing.
Different clinical studies have already shown the promising potential of using radiation therapy with immunotherapy approaches, including the inhibition or activation of selected molecules using monoclonal antibodies (mAbs), such as anti-CD137 combined with radiation therapy and the checkpoint inhibitor anti-PD1, which mediated tumor rejection in a murine model of mammary carcinoma.
Also, using a Toll-like receptor (TLR) 9 agonist (which simulates the structure of pathogen-associated molecular patterns) with radiation therapy induced a systemic antitumor humoral response in a mouse model of lung adenocarcinoma, reducing the number of pulmonary metastases and improving median survival.
[adrotate group=”1″]
Further evidence has derived from preclinical studies combining radiation therapy and anti-CTLA-4 mAb, when mice implanted with breast carcinoma cells exhibited complete tumor regression at the primary tumor site upon treatment with combination therapy, a significant delay in tumor growth at secondary sites and an increase in CD4 and CD8 T cell responses.
“While RT has traditionally been considered only as local therapy, it is now clear that it has systemic effects, many of which lead to improvements in antitumor immunity. Furthermore, the absence of systemic immunosuppression makes RT an attractive adjuvant for combination with immunotherapy. (…) As knowledge of the synergistic effects of RT and immunotherapy increases, the translational use of this strategy for a variety of cancers will become more feasible and more available to patients”, the authors conclude in their study.