A new study entitled “Randomized Phase III Trial of Adjuvant Androgen Deprivation in Combination with High-dose Conformal Radiotherapy in Intermediate and High Risk Localized Prostate Cancer” presented at the American Society for Radiation Oncology’s (ASTRO’s) 56th Annual Meeting suggests that prostate cancer patients who receive high-dose radiation therapy (HDRT) followed by a longer period of hormone suppression therapy, or androgen deprivation therapy (ADT), have higher five-year biochemical, disease-free survival (bDFS) and overall survival rates compared to patients who receive HDRT and a shorter duration of ADT.
A new study entitled “Randomized Phase III Trial of Adjuvant Androgen Deprivation in Combination with High-dose Conformal Radiotherapy in Intermediate and High Risk Localized Prostate Cancer” presented at the American Society for Radiation Oncology’s (ASTRO’s) 56th Annual Meeting suggests that prostate cancer patients who receive high-dose radiation therapy (HDRT) followed by a longer period of hormone suppression therapy, or androgen deprivation therapy (ADT), have higher five-year biochemical, disease-free survival (bDFS) and overall survival rates compared to patients who receive HDRT and a shorter duration of ADT.
Prostate cancer cells typically require androgen hormones such as testosterone to grow, and so ADT is usually recommended for patients suffering with prostate cancer. Radiation therapy (RT) together with ADT is a standard of care for patients with locally advanced prostate cancer.
The study presented at ASTRO enrolled 362 patients at 9 cancer centers in Spain, in order to assess if HDRT combined with long-term androgen deprivation (LTAD) therapy for 28 months was associated with better patient outcomes when compared to HDRT combined with short-term ADT (STAD) for four months.
The patients studied suffered from cT1c – T3aN0M0 prostate cancer with no metastasis, and had prostate specific antigen (PSA) levels of less than 100 ng/ml. Both groups received four months of neoadjuvant ADT + HDRT, with a median RT dose to the prostate of 78 Gy.
Patients were then randomly assigned to two groups either receiving adjuvant Goserelin (a luteinizing hormone that suppresses production of testosterone) subcutaneously for 24 additional months (LTAD) or receiving only four months of ADT (STAD).
The study’s primary endpoints were set to bDFS and toxic side effects.
[adrotate group=”1″]
A total of 11 patients in the LTAD group and 15 patients in the STAD group had bDFS, and after a median follow-up of 63 months, the five-year bDFS was significantly higher in the LTAD group (89.8%) compared to the STAD group (81.3%).
Furthermore, metastasis free survival (MFS) and overall survival (OS) was significantly higher in the LTAD group (93.6% and 94.8%) when compared to the STAD group (83.4% and 86.1%).
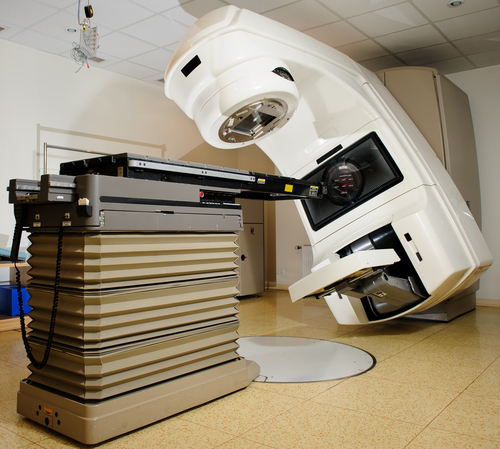
“The management of patients with intermediate- and high-risk prostate cancer is highly challenging. The clinician must choose the type of local treatment as well as the optimal timing and sequence of hormone therapy. Moreover, rapid and ongoing advances in treatment options require that physicians consider options that can impact both survival and quality-of-life. The five-year results of our study show that the combination of high-dose external radiotherapy utilizing new technologies, such as IMRT, VAMT and IGRT, and 28 months of hormone therapy are a very successful combination to achieve positive prostate cancer control. Of paramount consideration, LTAD therapy in combination with HDRT provides good quality of life through a non-invasive, safe and efficient treatment approach for patients with high-risk prostate cancer,” lead study author Almudena Zapatero, MD, PhD, a radiation oncologist at Hospital Universitario de la Princesa in Madrid Spain said in an ASTRO press release.