 In a new study entitled “Lipid and Metabolite Deregulation in the Breast Tissue of Women Carrying BRCA1 and BRCA2 Genetic Mutations” researchers showed the ability to detect metabolic changes in breast cancer patients (positive for BRAC gene mutations) using magnetic resonance spectroscopy. The study was published in the journal Radiology.
In a new study entitled “Lipid and Metabolite Deregulation in the Breast Tissue of Women Carrying BRCA1 and BRCA2 Genetic Mutations” researchers showed the ability to detect metabolic changes in breast cancer patients (positive for BRAC gene mutations) using magnetic resonance spectroscopy. The study was published in the journal Radiology.
The first genes whose defects were implicated in breast cancer were BRCA1 and BRCA2. It is now well established that women who carry mutations in BRAC genes have between a 45% and 90% increased risk of developing cancer (mutations in BRCA genes account for less than 3% of all breast cancers). Notably, cancer risk from a BRCA gene mutation is so high that women carrying these defects undergo preventive mastectomy (surgery to remove a breast).
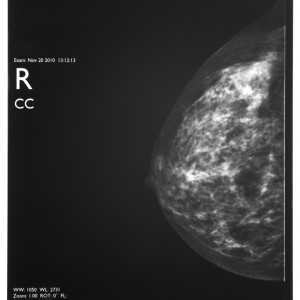
Due to the fact that women who carry BRCA mutations can develop cancer even after negative results determined by standard screening techniques, including mammography, magnetic resonance (MR) imaging, or ultrasonography (US), the authors hypothesized that pre-invasive states may occur but are not detected by these current methods.
[adrotate group=”1″]
In the present study, the research team wanted to understand whether carriers of BRCA gene mutations exhibited altered biochemical signatures in their mammary tissues characteristic of very early stages of cancer before any invasive state. To determine these metabolic changes, the team applied a technique called 2-D localized correlated spectroscopy (L-COSY) in women with BRCA1 (n=9) and BRCA2 (n=14) mutations and compared it to healthy controls (n=10) who lacked a family history of breast cancer. Standard screening techniques, such as MRI and ultrasonography were also applied.
The team found that while MRI and ultrasound detected no abnormal changes, L-COSY MRS identified significant biochemical changes in the breast tissue of women carrying BRCA1 and BRCA2 mutations, when compared to the control group, which could characterize a pre-invasive state. Additionally, the authors discovered significant alterations in lipid pathways among BRCA mutation carriers. However, the alterations were different between women with BRCA1 or BRCA2 mutations, with the latter exhibiting increased cholesterol levels (47%).
The authors highlight that their findings, if translated to larger populations, will allow women carrying BRCA gene mutations to monitor the biochemical changes in breast tissue that could potentially alert for pre-invasive changes. Further studies are necessary to confirm these findings and how they can impact cancer progression.
Carolyn Mountford, M.Sc., D.Phil., from the University of Newcastle in Callaghan, Australia, Brigham and Women’s Hospital in Boston and the Translational Research Institute in Brisbane, and study lead author commented in a press release, “These changes appear to represent a series of early warning signs that may allow women to make informed decisions as to when and if they have prophylactic mastectomy.”


