 Researchers associated with the Radiation Therapy Oncology Group (RTOG), a national clinical trials cooperative group, have recently reported that, compared to observation, radiation therapy is more effective in terms of recurrence prevention of ductal carcinoma in situ (DCIS) than previously thought. The study is entitled “RTOG 9804: A Prospective Randomized Trial for Good-Risk Ductal Carcinoma in Situ Comparing Radiotherapy with Observation” and was published in the Journal of Clinical Oncology.
Researchers associated with the Radiation Therapy Oncology Group (RTOG), a national clinical trials cooperative group, have recently reported that, compared to observation, radiation therapy is more effective in terms of recurrence prevention of ductal carcinoma in situ (DCIS) than previously thought. The study is entitled “RTOG 9804: A Prospective Randomized Trial for Good-Risk Ductal Carcinoma in Situ Comparing Radiotherapy with Observation” and was published in the Journal of Clinical Oncology.
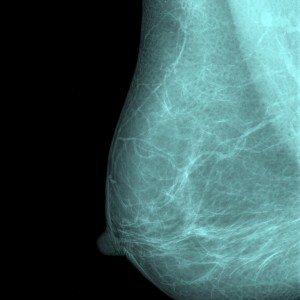
DCIS is the most common type of non-invasive breast cancer, which starts within milk ducts but does not spread into the surrounding breast tissue. DCIS by itself is not life-threatening, but it can increase the risk for invasive breast cancer and therefore requires treatment.
In 1998, when the RTOG study was started, radiation therapy was acknowledged to decrease the risk of recurrence for patients with DCIS by half. The RTOG 9804 study was conceived to determine the benefits of radiation therapy after breast-conserving surgery in comparison with patient observation in women who had “good risk” disease. The criteria for good-risk DCIS were: no evident cancer symptoms prior to the diagnose (detection usually by a mammogram), low or intermediate grade DCIS, and cancers no larger than 2.5 cm in diameter with margins of 3 mm or greater. The RTOG trial (1998 – 2006) was randomized and included 636 women found to have low- or intermediate-grade DCIS with good-risk characteristics.
[adrotate group=”1″]
Researchers found a surprisingly low rate of recurrence in patients submitted to radiation therapy, which was statistically significant in comparison with patients from the observational group. “This is an interesting study for two reasons,” explained Dr. Alan Hartford at Dartmouth’s Norris Cotton Cancer Center and one of the study’s authors in a news release. “First, it gives us an important group of baseline data about DCIS recurrence for patients who forego radiotherapy that shows a five-year risk of recurrence at 3.5% and nearly 7% at seven years. We will need to watch the following years closely. Secondly, if a patient did choose to have radiation therapy, that risk fell to 0.4% at five years and 0.9% at seven years.”
“For patients, the findings are useful as they consider whether to choose radiation therapy or not,” added Dr. Hartford. “If a woman presents with good-risk DCIS, maybe it’s not unreasonable for her to forego radiation therapy to avoid side effects and potential complications. However, these data are still young, and it is possible the risks of recurrence will continue to rise after seven years. The other reading is that radiation therapy substantially reduces the risk of recurrence for patients with good-risk DCIS, down to below 1% at seven years. This is a dramatic improvement.”
However, Dr. Hartford is cautious and notes that the low rate of recurrence in the treatment group could be off due to random chance and that the real risk might be somewhat higher.


