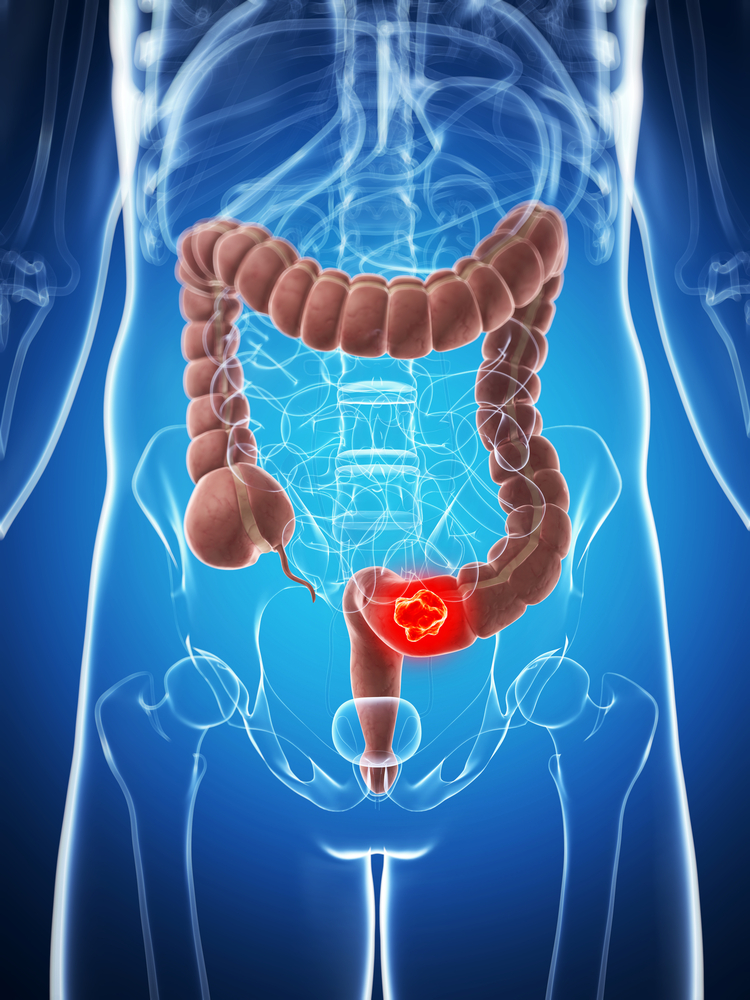
A new study examined secondary efficacy endpoints of preoperative radiation therapy (RT) in patients with advanced rectal cancer. The trial determined that patients who receive preoperative RT with irinotecan plus capecitabine have a four-year overall survival rate (OS) of 85%, and those who receive preoperative RT with oxaliplatin plus capecitabine have a four-year OS of 75%.
A new study examined secondary efficacy endpoints of preoperative radiation therapy (RT) in patients with advanced rectal cancer. The trial determined that patients who receive preoperative RT with irinotecan plus capecitabine have a four-year overall survival rate (OS) of 85%, and those who receive preoperative RT with oxaliplatin plus capecitabine have a four-year OS of 75%.
The study entitled “Efficacy Endpoints of Radiation Therapy Group Protocol 0247: A Randomized, Phase 2 Study of Neoadjuvant Radiation Therapy Plus Concurrent Capecitabine and Irinotecan or Capecitabine and Oxaliplatin for Patients With Locally Advanced Rectal Cancer”, was recently published in the International Journal of Radiation Oncology, the journal of American Society for Radiation Oncology (ASTRO).
This study is a secondary endpoint analysis of the Radiation Oncology Group (RTOG 0247) study, preformed in 2012, which reported that patients who were treated with preoperative RT with capecitabine plus oxaliplatin were able to achieve a complete remission of 21% whereas those treated with preoperative RT with capecitabine plus irinotecan only achieved 10%.
RTOG 0247 was a Phase II multi center clinical trial that enrolled 104 patients with advanced T3 and T4 rectal cancer. The clinical trial evaluated two chemotherapy regimens, with patients in one arm receiving capecitabine (dosing of 1200 mg/m2/d Monday to Friday) plus irinotecan (dosing of 50 mg/m2/wk for four weeks), and patients in the other arm receiving capecitabine (dosing of 1650 mg/m2/d Monday to Friday) plus oxaliplatin (dosing 50 mg/m2/wk for 5 weeks).
Surgery was performed 4 to 8 weeks following chemoradiation, then after 4 to 6 weeks, patients in both study arms received adjuvant chemotherapy (oxaliplatin 85 mg/m2; leucovorin 400 mg/m2; 5-fluorouracil 400 mg/m2; 5-fluorouracil 2400 mg/m2) every 2 weeks for a total of nine weeks.
Univariate analysis with the Kaplan-Meier method was used to determine Disease-free survival (DFS) and overall survival (OS). The cumulative incidence method was sued to estimate Local–regional failure (LRF), distant failure (DF), and second primary failure (SP).
[adrotate group=”1″]
The results revealed that, after a median follow-up period of four years DSF, OS, LRF, DF and SP estimation were 68%, 85%, 16%, 24% and 2%, respectively for the capecitaine plus irinotecan group. For the capecitabnie plus oxaliplatin group the estimations were of 62% (DSF), 75% (OS), 18% (LRF), 30% (DF) and 6% (SP).
In a recent news release, Neal J. Meropol, MD, co-author of the study, and the Dr. Lester E. Coleman Jr., Professor of Cancer Research and Therapeutics and chief of the Division of Hematology and Oncology at University Hospitals Case Medical Center and Case Western Reserve University in Cleveland said “Our new analysis of RTOG 0247 provides us with favorable efficacy results of two preoperative chemotherapy regimens used in conjunction with radiation therapy protocols. These favorable long-term survival rates confirm that both of these concurrent chemoradiotherapy regimens followed by surgery can be a highly curative approach for patients with localized rectal cancer, despite the low pCR results we reported in 2012. It is important to find new biomarkers beyond the local remission rate that can help us determine which patients will be cured and who may benefit from more aggressive therapy following chemoradiation.”