 In a recent article titled “STING-Dependent Cytosolic DNA Sensing Mediates Innate Immune Recognition of Immunogenic Tumors”, published in Immunity, a team of researchers from the Ludwig Institute for Cancer Research, Chicago, has found the main signaling mechanisms and cellular interactions responsible for initiating an immune response in tumors receiving radiation therapy.
In a recent article titled “STING-Dependent Cytosolic DNA Sensing Mediates Innate Immune Recognition of Immunogenic Tumors”, published in Immunity, a team of researchers from the Ludwig Institute for Cancer Research, Chicago, has found the main signaling mechanisms and cellular interactions responsible for initiating an immune response in tumors receiving radiation therapy.
“Much of the conversation about the mechanisms by which radiation kills cancer cells has historically focused on the damage it does to DNA,” study author Ralph Weichselbaum, co-director of the Ludwig Center at the University of Chicago, said in a press release. “But it has recently become increasingly clear that the immune system plays an important–perhaps central–role in destroying tumors subjected to radiotherapy. Our study shows how radiation, DNA damage and the immune response that follows are linked.”
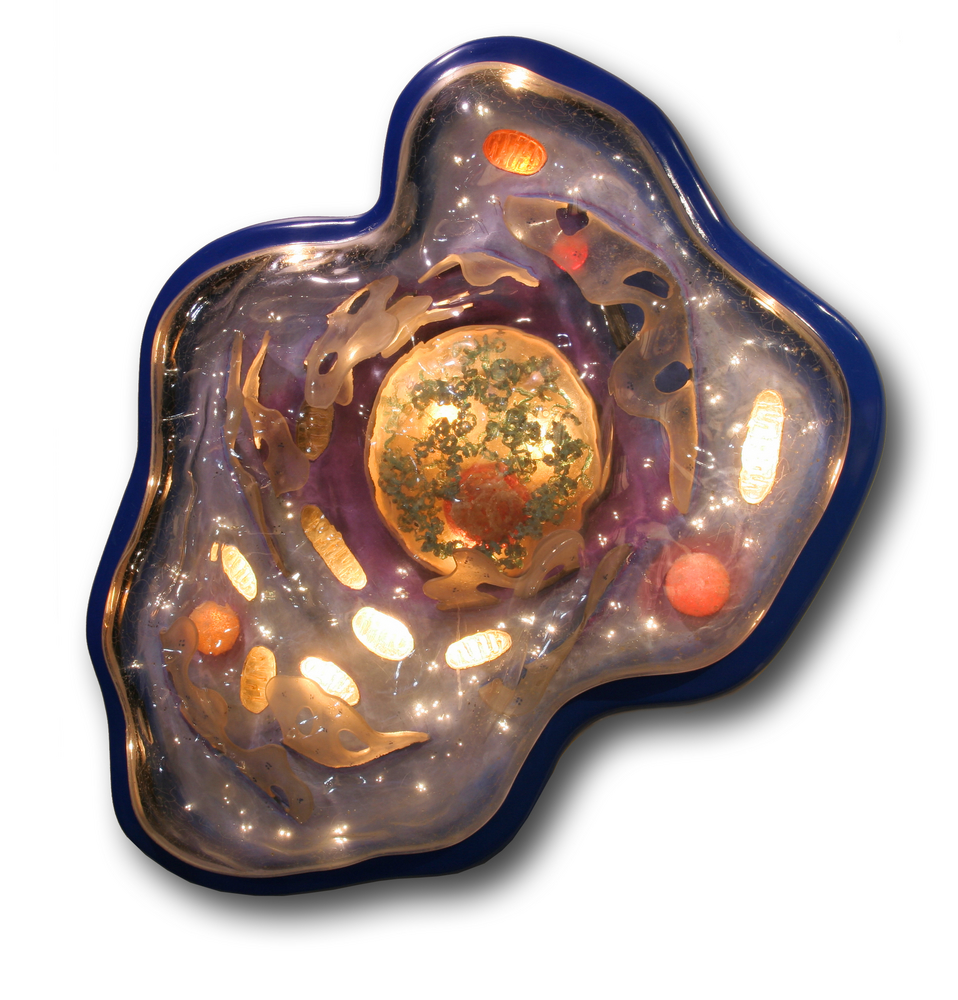
The team observed that within the innate immune system, dendritic cells (DCs) are key players in this phenomenon. Using mice models and in vitro cellular essays, researchers were able to demonstrate that a protein within DCs, named STING, is essential in the activation of an immune response towards irradiated tumors, detecting minor tumor DNA fragments and allowing the production of the immune cytokine interferon-β (IFN-β). This in turn enables the activation of CD8 T cells, that have the ability to recognize and kill cancer cells.
Throughout DCs immune surveillance, these cells use an array of biochemical sensors that can recognize different types of pathogens. One of these detectors, an enzyme named cGAS, can be activated upon sensing of double-stranded DNA fragments, including damaged DNA that is shed from irradiated cells. This allows the immune system to mount an effective immune response against irradiated tumors.
“This seems to be a fairly specific response in the context of radiation. If you knock out the STING gene in mice, their tumor growth is similar to that of normal mice. But, in the knock-out mice, the tumors are far more resistant to radiation than the tumors of control mice”, Dr. Weichselbaum added.
[adrotate group=”1″]
The results showed that DCs from transgenic animals that did not produce STING, were unable to activate CD8 T cells after tumor irradiation. This capacity could be reverted upon addition of IFN-β.
Furthermore, DCs from animals that were modified to loose the expression of cGAS genes, also failed to activate CD8 T cells.
Additionally, mice carrying tumors and injected with STING-activating molecules became more sensitive to radiation treatment.
“These findings could open the door to improving cancer therapy. Drugs that activate STING signaling or the induction of IFN-β could be used to boost the effects of radiotherapy on tumors. Those effects might be observed in chemotherapy as well, since it too causes significant DNA damage,” Dr. Weichselbaum concluded.