 Researchers from the University of Florida Proton Therapy Institute have published favorable clinical outcomes of a prospective phase 2 study of consolidative involved-node proton therapy (INPT) as a combined therapy for patients with stage I to III Hodgkin lymphoma (HL), a type of cancer which originates from a particular kind of white blood cells, the lymphocytes.
Researchers from the University of Florida Proton Therapy Institute have published favorable clinical outcomes of a prospective phase 2 study of consolidative involved-node proton therapy (INPT) as a combined therapy for patients with stage I to III Hodgkin lymphoma (HL), a type of cancer which originates from a particular kind of white blood cells, the lymphocytes.
Treatment for HL is dependent on the age and sex of the patients and also on the stage, bulk, and histological subtype of the disease. Radiation therapy, chemotherapy or hematopoietic stem cell transplantation are all viable options.
However, several HL patients treated with the current regime of radiotherapy and chemotherapy suffer from late effects, including the onset of breast cancer or heart disease.
Proton therapy is believed to be a superior form of radiation therapy, since it is able to provide superior dose distribution and a more precise delivery of photons, allowing the radiation oncologist to increase the dose to the tumor while reducing the dose to surrounding normal tissues, diminishing potential harmful side effects and increasing the direct impact on the tumor as well as tumor control.
The research team, led by radiation oncologist Bradford Hoppe, PhD, did a 4-year follow up of 15 patients with newly diagnosed HL who received INPT directed at tumor-bearing lymph nodes after completing chemotherapy.
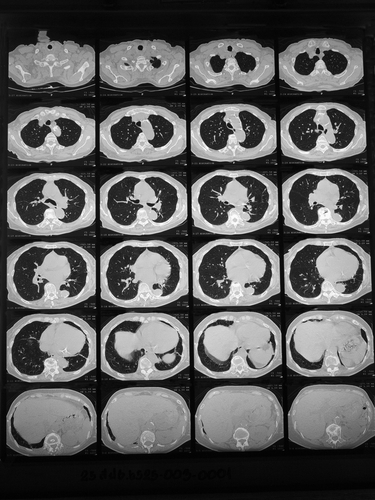
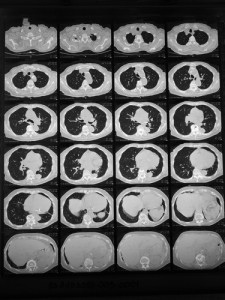
Based on 18F-Fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) response, five children received 15 to 25.5 cobalt Gy equivalent (CGE) of INPT after four cycles of chemotherapy, and 10 adults received 30.6 to 39.6 CGE of INPT after three to six chemotherapy cycles.
The scientists then compared the dosimetric impact of proton therapy with that from intensity-modulated radiation therapy (IMRT) and 3D conformal radiotherapy (3D CRT).
The results demonstrated statistically significant and clinically relevant reductions in radiation dose to non-target tissue. Furthermore, proton therapy clearly reduced treatment toxicity, with protons reducing the average integral body dose by 49% compared with IMRT and by 57% compared with 3D CRT, with an additional reduction of the dose to specific organs-at-risk. The mean heart dose was lowered by 7.6 Gy (46%) and by 3.3 Gy (27%) compared with 3D CRT and IMRT, while the mean lung dose was reduced by 4.5 and 2.7 Gy compared with 3D CRT and IMRT, respectively.
Among women, proton therapy reduced the mean breast dose by an average of 2.1 and 1.7 Gy, compared with 3D CRT and IMRT.
Proton therapy regime also exhibited comparable control rates to those expected with conventional radiation treatment, with data showing a three-year relapse-free rate of 93% and a three-year event-free rate of 87%. Additionally, no patients developed grade three or higher toxicity during follow-up.
[adrotate group=”1″]
Although several dosimetry studies have previously reported proton therapy’s ability to reduce dose to the heart, breast and lungs in Hodgkin lymphoma patients, this study was the first to actually treat patients with proton therapy.
“All 15 patients derived benefits from using proton therapy,” said Dr. Hoppe. “The results show that the use of protons, as opposed to similar conventional photon therapy, reduced the risk of long-term side effects by reducing or eliminating radiation doses to healthy tissue without compromising the cure rate.”
The results from this study offer novel insights regarding the use of proton therapy after chemotherapy with reduced radiation dose outside of the target area, potentially reducing the risk of radiation-induced late effects.