 Malignant tumors arising within the nasal cavity and paranasal sinuses are rare and composed of several histological types, making controlled clinical trials to establish the best treatment difficult. Although surgery is the primary treatment for early-stage resectable sinonasal cancers, radiation therapy is necessary as adjuvant therapy in advanced disease and as primary therapy for unresectable cancers or for patients who are not candidates for surgery.
Malignant tumors arising within the nasal cavity and paranasal sinuses are rare and composed of several histological types, making controlled clinical trials to establish the best treatment difficult. Although surgery is the primary treatment for early-stage resectable sinonasal cancers, radiation therapy is necessary as adjuvant therapy in advanced disease and as primary therapy for unresectable cancers or for patients who are not candidates for surgery.
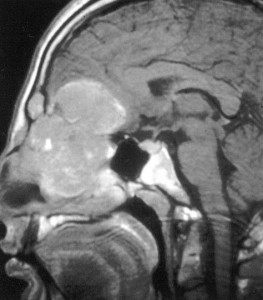
These tumors are anatomically close to the vital structures of the brain, eyes, cranial nerves and optic pathways, thus the unique physical properties of charged-particle therapy which deposits energy (from carbon ions or protons) far more selectively than X-rays, could allow clinicians to fine-tune the dosage and improve tumor control and survival.
A team of researchers from the Mayo Clinic, Rochester, Minnesota, undertook a systematic review and meta-analysis to compare the clinical outcomes of patients treated with charged particle therapy with those of individuals receiving photon therapy, in an attempt to understand if the former provides better outcomes than traditional forms of radiotherapy.
The scientists analyzed more than 1,400 patients from 41 non-comparative studies of nasal cavity and paranasal sinus tumours present in biomedical databases that included treatment-naive cohort (both primary and adjuvant radiation therapy) and those with recurrent disease, with overall survival, disease-free survival and locoregional control being the primary outcomes of interest at 5 years and at longest follow-up.
At 5 years, disease-free survival was significantly higher for charged particle therapy than for photon therapy, however, at longest follow-up, this event rate did not differ between groups. Additionally, locoregional control did not change between treatment groups at 5 years although it was higher for charged particle therapy than for photon therapy at longest follow-up.
In a subgroup analysis, the researchers compared the two major techniques from each group — proton-beam therapy and intensity-modulated radiation therapy (IMRT) — concluding that disease-free survival was significantly better with proton-beam therapy than with IMRT at 5 years, alongside locoregional control at the longest follow-up.
Particle therapy seems to be the best choice for base-of-skull tumors, however, the fact that the trials studied were not randomized and that a higher proportion of patients with high-risk histologic types were treated with photon therapy than with charged-particle therapy (50% vs 27%) can constitute a selection bias in the study, said Piet Dirix, MD, PhD, from the Iridium Cancer Network in Wilrijk, Belgium. However, there was also a higher proportion of patients with recurrent previously treated disease and advanced disease in the charged-particle group, confirmed senior investigator Robert Foote, MD, from the Mayo Clinic.
[adrotate group=”1″]
The current number of proton therapy centers is very limited, with the majority of patients in this study receiving charged-particle therapy in just 3 centers – the Massachusetts General Hospital in Boston, the National Cancer Center Hospital East in Chiba, Japan and the Hyogo Ion Beam Medical Center in Japan – in contrast to patients receiving photon therapy, who were treated at a variety of centers in several different countries.
Although charged-particle therapy is rising in the United States, where multiple proton-beam therapy centers are under construction, there is some criticism pointing that this kind of treatment is being hyped and that it sells hope without clear benefits for the patients. Additionally, it is far more expensive than other forms of radiotherapy, one of the reasons why some private medical insurers have stopped reimbursing proton-beam therapy for prostate cancer.
Despite these issues the present study, published in the peer-reviewed journal The Lancet Oncology seems to indicate that compared with photon therapy, charged particle therapy could be associated with better outcomes for patients with malignant diseases of the nasal cavity and paranasal sinuses, an encouraging perspective that should be addressed in future research.


