 A study published by the American Journal of Managed Care that examined the impact of health insurance and other social factors on the prescribed treatment for breast cancer in Florida between 1997 and 2002 suggests that for different types of health systems and social conditions there are different treatment responses.
A study published by the American Journal of Managed Care that examined the impact of health insurance and other social factors on the prescribed treatment for breast cancer in Florida between 1997 and 2002 suggests that for different types of health systems and social conditions there are different treatment responses.
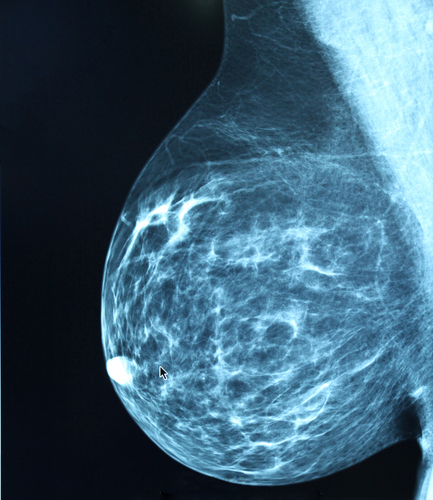
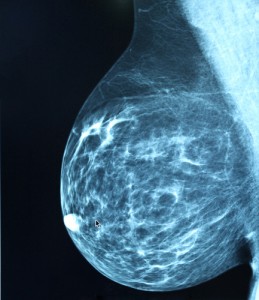
According to information available in the study, breast conservative surgery (BCS) combined with radiotherapy (RT) has become a standard recommended treatment for early-stage breast cancer since the 1990s, as it has similar results to mastectomy, while preserving the breast. BCS combined with RT is recommended by The National Institutes of Health Consensus Development Conference on Treatment of Early-Stage Breast Cancer as the appropriate therapy for stage 1 and stage 2 breast cancer with similar surviving rates of mastectomy. However, the number of mastectomies between 1997 and 2002 was higher than BCS and RT combination, represented by 58.62% and 38.61% respectively. In addition, data also showed that only 47.45% of women receiving BCS also underwent RT, even though almost 80% of women with early-stage breast cancer fit the criteria to receive it according to the American College of Radiology. Nationwide, data showed that only 38% to 65% of the patients chose RT.
The analysis also pointed out that the number of deaths related to breast cancer have also been declining since 1990 due to earlier detection, a factor attributed to the success of the treatment, the circumscription of the tumor, and to more effective treatments. Women treated for localized breast cancer are more likely to survive than women treated for late-stage cancer.
Using these data points, the authors of the recent study sought to determine if health insurance and social factors influenced the type of treatment women are ultimately given.
In the observed group, most women were age 60 years or older (68.18%), married (57.65%), and non-Hispanic/white (86.07%). The distribution of women by health insurance type was 31.54% privately insured, 1.74% Medicaid, 50.12% Medicare, 14.07% other, and 2.54% uninsured. The majority of women (58.62%) received BCS, while 38.61% had a mastectomy and 2.77% had no surgery. Of those who received BCS, only 47.45% received RT following BCS. Overall, 27.81% women received BCS with RT.
[adrotate group=”1″]
Analyzing health systems, the authors observed that most of the women with private (61.67%), Medicare (57.22%), and other (60.24%) insurance received BCS. The percentage of women who received BCS among Medicaid insured and uninsured women was less than 50% (47.18% and 47.13%). Moreover, the number of women who received RT after BCS was similar for those insured by Medicaid and those uninsured (41.30% and 40.94%, respectively) and lower compared with women insured privately (45.93%), through Medicare (47.87%), and through other government programs (51.05%).
Testing social factors, researchers seem to have observed that single, divorced, or widowed women were less likely to receive BCS with RT compared with married women. At the same time, younger women were less likely to receive BCS and RT, a tendency changed above 70 years old.
Finally, the size of the tumor also seems to influence the type of chosen treatment. Patients with a tumor 2 cm or larger had significantly lower chances of having RT after BCS.